 The breast cancer awareness movement is important. It could be a lot better. It fails to tell women about their most important natural defense against breast cancer.
The breast cancer awareness movement is important. It could be a lot better. It fails to tell women about their most important natural defense against breast cancer.
Breast Cancer Awareness Factors
Good summaries of the most popular factors are publicized on the Susan G. Komen website. Two categories are seemingly comprehensive. The first is:
Factors Affecting Breast Cancer
This page provides an extensive list of such factors, with links to explanations about what they entail: Factors That Affect Breast Cancer Risk.
This is the complete list:
- Age
- Age at First Childbirth and Number of Childbirths
- Age at First Period
- Age at Menopause
- Alcohol
- Ashkenazi Jewish Heritage
- Being Female
- Birth Control Pill Use
- Blood Androgen Levels
- Blood Estrogen Levels
- Body Weight and Weight Gain
- Bone Density
- Breast Density on Mammogram
- Breastfeeding
- Exercise (Physical Activity)
- Family History of Breast, Ovarian or Prostate Cancer
- Fruits, Vegetables and Carotenoids
- Height
- Hyperplasia and Other Benign Breast Conditions
- Inherited Gene Mutations
- Light at Night and Shift Work
- Lobular Carcinoma in Situ (LCIS)
- Menopausal Hormone Therapy (Postmenopausal Hormone Use)
- Personal History of Breast Cancer or Other Cancers
- Prolactin Hormone Levels
- Race and Ethnicity
- Radiation Exposure in Youth
Factors Under Study
This page provides a list of current research areas, with links to explanations of each item. This list represents what the medical research is looking at right now. See the explanations here: Factors Under Study.
This list is as follows:
- Acrylamide (found in foods such as French fries)
- Antibiotic Use
- Anti-depressant Use
- Aspirin Use
- Birthweight
- Breast Size
- Breastfed as an Infant
- Dairy Products
- Breast cancer after menopause
- Breast cancer before menopause
- Diabetes and Insulin
- Dietary Fat
- High-fat diet during the teenage years
- Fertility Drugs
- Folic Acid (Folate) and Multivitamin Use
- Insulin-like growth factor 1 (IGF-1) hormone levels
- Meat consumption
- Moles (on the skin)
- Parabens (found in some body care products and cosmetics)
- Plastics and bisphenol A (BPA)
- Plastics
- Secondhand smoke exposure (passive smoking)
- Smoking
- Soy and phytoestrogens
- Stress
- Vitamin D
Peeling Back the Onion
Wow…that is quite a boatload of information. Let’s take a look at what all this might mean.
Imagine that the factors in both lists represent the layers of an onion – i.e., each factor peels back to reveal further details of what underlies it.
Unfortunately, in keeping with this analogy, none of these factors gets to the core of the onion, meaning a clear explanation of the causes of breast cancer. The vast majority of research, in fact, is heading nowhere of consequence.
The basis for that claim is this:
Modern medicine does not have a cure for breast cancer.
As of August, 2022, PubMed lists nearly 325,000 research articles on breast cancer.
Nearly 325,000 articles without discovering causes or cures for breast cancer!
THIS IS A MAJOR DISAPPOINTMENT
Now for Some Good News
Let’s look under the hood of just one of the factors under study and see if we can find something useful. (Of course we can. That’s why I am writing this post in the first place.)
That factor is vitamin D.
A link on the Factors Under Study page (see above) expands out to the mainstream perspective on this topic, here: Vitamin D – How much is enough?
You may want to read it just to get the party line on vitamin D. If you want a one-word summary of the current medical perspective, though, here is how modern medicine views the issue of vitamin D vs breast cancer: iffy.
The good news is that mainstream medicine is beginning to point in the right direction. At least a little bit. Sort of. Maybe. (Okay, not so much.)
For starters, take a look at the introductory paragraph on the vitamin D page linked above:
There has been much scientific interest in whether vitamin D impacts cancer risk. In November 2010, the Institute of Medicine (IOM) released a report—Dietary Reference Intakes for Calcium and Vitamin D—updating its dietary recommendations for vitamin D. The IOM reviewed the scientific evidence and found while vitamin D was important to bone health, it remains unclear whether it has other health benefits. Although some studies have suggested a protective link between vitamin D and many types of cancer, including breast cancer, vitamin D is not currently recommended for cancer or chronic disease prevention [my bolding]. However, this is an active area of research and a growing number of studies are looking at whether vitamin D might lower the risk of breast cancer.
Not exactly a ringing endorsement.
The Conundrum
What we have is a mainstream view that fails to understand the real biology of vitamin D. This failure is at the root of a conundrum.
Consider that just a little digging into the connection between breast cancer and vitamin D reveals this:
of breast cancer and the highest mortality rates caused by breast cancer.
In the face of such observations, why is modern medicine’s take on vitamin D vs. breast cancer so iffy?
THE GOOD NEWS IS … We can clear up the puzzle when we understand where we get vitamin D and how we use it.
A Different Perspective
Let’s start by examining the incidence of breast cancer that is depicted in the following graph:
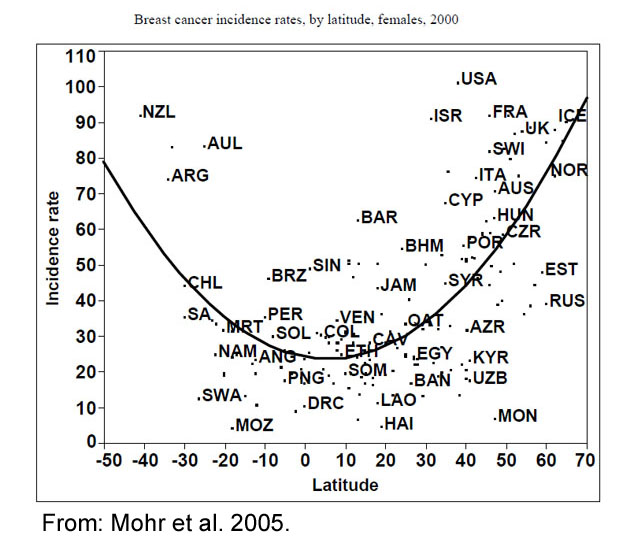
This graph shows the incidence of breast cancer in 175 countries relative to their distance from the equator. In the northern hemisphere, the highest cancer rates were found in Norway, Iceland, Sweden, and Canada. These countries are all located above 50o North latitude.
(We will talk about why the U.S. is a high-incidence outlier below.)
In contrast, the lowest incidences of breast cancer occurred in countries within 20o North or South latitude. This list included Haiti, Mozambique, Rwanda, and Malawi.
So far, this is the most thorough survey of latitude vs. breast cancer worldwide. However, it is not a new idea. One of the first such surveys, published in 1990, showed that the incidence of fatal breast cancer in the U.S. increased with latitude. Northern areas (New York, Chicago) were associated with up to a 1.8-fold higher rate of mortality in comparison with southern areas (Phoenix, Honolulu).
Also in 1990, a parallel study of breast cancer incidence in the former Soviet Union showed the same trend as in the U.S.
Taking a slightly different angle, a study in 2014 found that breast cancer patients had an improved chance of survival when diagnosed in summer versus winter.
What Does All This Mean?
Here is what we know so far:
- The incidence of breast cancer increases with increasing latitude.
- The incidence of breast cancer increases with decreasing levels of vitamin D.
- Vitamin D levels decrease with increasing latitude.
- Assuming* that vitamin D, therefore, acts to prevent breast cancer, taking more more vitamin D should help.
- Unfortunately, research DOES NOT clearly and consistently show that increasing the intake of vitamin D reduces the incidence of breast cancer.
*Keep in mind that associations between factors cannot prove that one causes the other.
In other words – DANG! – what we have is a seemingly great idea that is not supported by experimental studies.
The Missing Ingredients
Medical researchers, bless their hearts, have almost figured it out. Getting the ultimate answer, though, requires some digging into the physiology of vitamin D.
What we find is that the above graph is an association with sunshine, particularly UVB light. This is the portion of sunshine that drives the formation of vitamin D in our skin.
dietary or supplementary vitamin D!
Oral Vitamin D: Not All It’s Cracked Up To Be
Oral vitamin D refers to whatever you consume in foods or as supplements. In the D3 form, it helps to regulate calcium metabolism and to direct where calcium should be going. It clearly has benefits for bones and teeth. (This does not include the D2 form that we get from mushrooms and plants.)
Note that we have no feedback mechanism for oral vitamin D3. This means that we do not sense its presence as a way to regulate its function. The lack of a feedback mechanism can lead to errors in shuttling calcium. One result of such errors is the accumulation of calcium deposits in arteries, in the pineal gland, in the placentas of pregnant women, and in many other areas of our bodies.
Just one of the consequences of this wayward process is cardiovascular disease caused by clogged and hardened arteries.
This is only one possible outcome from oral vitamin D when it goes haywire. Many other variables are in play, such as levels of calcium, vitamin K2, magnesium, and boron.
The main point is that raising your own level of vitamin D by supplementing with vitamin D3, or consuming foods fortified with it, may or may not give you the health benefits that you expect. In fact, probably not.
Why Does This Happen?
Vitamin D is a hormone. Hormones are carefully regulated and interdependent among multiple factors. We are not meant to overload our bodies with excess hormones. Doing so disrupts what should be a carefully balanced set of nutrients and other hormones.
The Best Vitamin D: Guaranteed
You know that sunshine on your skin drives the formation of vitamin D. What you may not know is that the product of this synthesis is vitamin D sulfate.
Vitamin D sulfate is made from common substance in your skin: cholesterol.
Adding the sulfate to a cholesterol precursor requires cellular energy. The only source of energy that works for this synthesis is UVB light. Except for mother’s milk (and unpasteurized cow’s milk), there are no dietary or supplementary sources of vitamin D sulfate.
Furthermore, our bodies do not make vitamin D sulfate from oral vitamin D.
Vitamin D sulfate – naturally made in your skin in the presence of UVB light – is the real force behind the health benefits of vitamin D.
PROTECTION AGAINST BREAST CANCER.
MAJOR flaw of the breast cancer awareness movement.
The U.S. Outlier
The high incidence of breast cancer in the U.S. is associated with many factors. All of them center around indoor living. Even the lowest incidences, found in southern states, are higher than those of near-equatorial countries.
The association between latitude and the incidence of breast cancer only reflects the potential for exposure to UVB light. Women living in sunny climates undermine the potential benefits of vitamin D sulfate by staying mostly indoors, by covering their skin when outdoors, or by wearing sunscreen.
In sunny Qatar, for example, women who fully cover themselves for religious reasons have some of the lowest recorded levels of vitamin D. Not surprisingly, breast cancer is the most common form of cancer in women in Qatar.
It is not unlike sunshine avoidance in the U.S., although for different cultural reasons.
Wait! There’s More!
Some scientists have begun to connect the dots for this issue. Perhaps the leading researcher worldwide is Dr. Stephanie Seneff of MIT. Her research focuses on vitamin D metabolism and health. According to Dr. Seneff, vitamin D sulfate is a key hormone for protection against cancer, for a stronger immune system, for better cardiovascular health, and for optimal brain function.
In other words, the benefits attributed to vitamin D are really due to vitamin D sulfate.
As Dr. Seneff points out, the key ingredients for making vitamin D sulfate are cholesterol, sulfur, and UV-B light. That’s all it takes.
Having enough of each ingredient is crucial for optimizing the amount of vitamin D sulfate that you can make. Here is what you must know about each one:
Cholesterol
This steroid is not the health bugaboo that mainstream medicine makes it out to be. We absolutely must have sufficient amounts of cholesterol for optimal health. It is the key precursor that we need for making vitamin D sulfate.
It should be no surprise that taking cholesterol-lowering drugs leads to a greater association with many kinds of cancer, including breast cancer.
Your body already makes most of the cholesterol that you need for good health. You can also benefit from consuming cholesterol-containing foods such as eggs, liver, shellfish, red meat, and cheese.
If you are worried about cholesterol as a health problem, you can find out the real truth behind this made-up issue in Malcolm Kendrick’s book, The Great Cholesterol Con: The Truth About What Really Causes Heart Disease and How to Avoid It.
Sulfur
Dietary sulfur most commonly comes from the two sulfur-containing amino acids in all proteins, methionine and cysteine. High sulfur-containing foods also include cole crops (broccoli, cauliflower, cabbage, kale, Brussels sprouts, turnips), allium vegetables (garlic, onions, leeks, chives), and eggs.
One of the simplest ways to get plenty of sulfur is to supplement with methyl sulfonyl methane (MSM). It is a widely available and inexpensive supplement. You can get all the sulfur you need from a daily teaspoon of MSM powder dissolved in a glass of water.
UV-B Light
As with fears about cholesterol, mainstream medicine has also perpetrated a scary dogma about ultraviolet light and skin cancer. Unfortunately, this dogma contradicts basic human biology. Your skin must be exposed to UVB light to make vitamin D sulfate.
in the presence of UVB light.
There is no better source of UV-B light than sunshine.
Getting enough UV-B light on your skin, however, can be tricky. In winter, the amount of UV-B light reaching the Earth’s surface beyond 40 degrees north or south latitude is too low to make enough vitamin D sulfate. Safe tanning beds or UV-B lamps can be helpful.
Getting enough exposure to UV-B light in summer is less of a problem. The highest levels occur between about 10:00 AM and 2:00 PM.
The amount that each person needs depends on several factors. Lighter skin requires less than darker skin. The best indicator for getting the right amount of exposure is a change in skin color to pinkish. The key is to stop at that point to avoid sunburn.
Resources
Badawi A, Arora P, Sadoun E, Al-Thani AA, Thani MH. 2012. Prevalence of vitamin D insufficiency in qatar: a systematic review. J Public Health Res. 1(3):229-235.
https://www.ncbi.nlm.nih.gov/pubmed/25170469
Garland FC, Garland CF, Gorham ED, Young JF. 1990. Geographic variation in breast cancer mortality in the United States: a hypothesis involving exposure to solar radiation. Prev Med 19:614-622.
https://www.ncbi.nlm.nih.gov/pubmed/2263572
Goldstein MR, Mascitelli L, Pezzetta F. 2008. Do statins prevent or promote cancer? Curr Oncol 15(2):76-77.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2365486/
Gorham ED, Garland FC, Garland CF. 1990. Sunlight and breast cancer incidence in the Soviet Union. Int J Epidemiol. 19(4):820-824.
https://www.ncbi.nlm.nih.gov/pubmed/2084008
Ho, A, Gabriel A, Bhatnagar A, Etienne D, Loukas M. 2014. Seasonality pattern of breast, colorectal, and prostate cancer is dependent on latitude. Med Sci Monit. 20:818-824.
https://www.ncbi.nlm.nih.gov/pubmed/24835144
Hwang JJ, Donnelly TT, Ewashen C, McKiel E, Raffin S, Kinch J. 2015. Sociocultural influences on Arab women’s participation in breast cancer screening in Qatar. Qual Health Res. Dec 1. [Epub ahead of print]
https://www.ncbi.nlm.nih.gov/pubmed/26631675
Mohr, SB, Garland CF, Gorham ED, Grant WB, Highfill RM, Garland FC. 2005. Mapping vitamin D deficiency, breast cancer, and colorectal cancer. Proceedings of the ESRI International User Conference, Redlands, CA. ESRI Vol. 1468.
http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.405.4511&rep=rep1&type=pdf
Seneff, S. 2014. Cholesterol, sulfate, and heart disease. Wise Traditions Workshop, London.
https://people.csail.mit.edu/seneff/London2014/SeneffHeartDisease2014.pdf
Seneff S, Davidson RM, Lauritzen A, Samsel A, Wainwright G. 2015. A novel hypothesis for atherosclerosis as a cholesterol sulfate deficiency syndrome. Theor Biol Med Model. May 27;12:9.
https://www.ncbi.nlm.nih.gov/pubmed/26014131
Weller RB. 2016. The health benefits of UV radiation exposure through vitamin D production or non-vitamin D pathways. Blood pressure and cardiovascular disease. Photochem Photobiol Sci. Dec 23. [Epub ahead of print]
https://www.ncbi.nlm.nih.gov/pubmed/28009890
Yao S, Kwan ML, Ergas IJ, Roh JM, Cheng TD, Hong CC, McCann SE, Tang L, Davis W, Liu S, Quesenberry CP Jr, Lee MM, Ambrosone CB, Kushi LH. 2016. Association of serum level of vitamin D at diagnosis with breast cancer survivial: A case-cohort analysis in the Pathways Study. JAMA Oncol. Nov 10. [Epub ahead of print]
https://www.ncbi.nlm.nih.gov/pubmed/27832250
All the best in natural health,
![]()
Statements on this page have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
Dear Dr. Clark,
I have been dealing with PHN for the past 7 months, particularly the itch issue. I tried to go to the sites suggested in some of your videos but they didn’t come up. So, basically, I’d love some direction about how to manage the itch / pain of PHN.
Thanks very much!
Hi, Alan:
This is an all too common issue that has been notoriously difficult to solve. I am sure that is not news to you. Nevertheless, a good place to start exploring a variety of alternative treatments would be here:
https://www.practicalpainmanagement.com/patient/conditions/postherpetic-neuralgia/alternative-treatments-postherpetic-neuralgia
Ice packs and capsaicin creams have also been used with some success. Good luck!
All the best,
Dennis