 Who needs a fructan intolerance remedy? Probably anyone with chronic gut pain, unexplained gas, bloating, or diarrhea. Here’s what you should know.
Who needs a fructan intolerance remedy? Probably anyone with chronic gut pain, unexplained gas, bloating, or diarrhea. Here’s what you should know.
Although you may benefit from a fructan intolerance remedy, it won’t address the underlying cause of your intolerance. Toward the end of this article I’ll explain what the REAL cause is and what you can do to overcome it.
Look, good food should be your friend. Preparing it and eating it should be enjoyable.
And once you finish a meal, you should feel great.
Then you can enjoy doing whatever your day has in store for you without digestive issues rearing their ugly heads.
If that’s not you, you may be suffering from what I call the ‘GI blues’? (Meaning, gastrointestinal issues, not the 1960 Elvis Presley movie, G.I. Blues.)
You know the feeling – general blahs that seem to start in your gut, rumbling gas and bloating, chronic diarrhea or constipation (or both!), nausea, or maybe even downright painful cramps.
It may even be so bad you find yourself depending on ‘tummy pills’ to get through the day (or night).
You’re not alone. In fact, meds for treating GI problems are the most commonly used medical treatments in the world.
Why such demand?
Start by looking at what you eat.
Could certain foods be shoving you down into GI purgatory?
You probably already know about one of the most common culprits – gluten-containing grains and foods made from them.
However, recent research reveals an additional food ingredient behind frequent digestive distress: fructans.
Gluten sensitivity, meet fructan intolerance.
The Fructan Surprise
First off, fructans are a two-sided health puzzle.
They can be very good for your health.
Or they can be very bad for your health.
Adding to the confusion, when fructans ‘go bad’, symptoms of fructan intolerance mimic those caused by glutens.
Sure, glutens get a lot of attention, deservedly so, for the digestive and other health problems they can cause.
However, estimates suggest at least a third of cases diagnosed as gluten sensitivity are actually caused by fructans.
Fructans and glutens are radically different kinds of ingredients. The challenge for anyone with chronic digestive problems is distinguishing between their respective types of intolerance.
And then, if it turns out to be from fructans, taking the right steps for reversing those issues.
Unfortunately, modern medicine doesn’t have a good handle on how to diagnose or overcome fructan intolerance.
Such failures rest on the simple-minded view that fructans cause health problems.
That view is incorrect, as you’ll learn later in this article.
Fructans: The New Kid on the Dietary Block
Figuring out whether you have a fructan problem starts with knowing what fructans are and where they come from in your diet.
Fructans are specific types of carbohydrates. (As opposed to glutens, which are proteins.)
The word root, ‘fruct’, tells you something about them already. It’s the same word root giving us the name of the ‘fruit’ sugar, fructose.
When applied to fructans, it refers to strings of fructose molecules hooked together into polymers. Fructans are thereby comprised mostly of chains of fructose. In addition, they typically include a core molecule of sucrose (table sugar).
The shorter chains (2-9 fructose molecules) are called fructo-oligosaccharides (FOS). Longer chains (60 or more fructose molecules) make up polysaccharides called inulins.
SIDENOTE: Fructan intolerance is not due to fructose. It’s due to an inability to digest fructose chains. We simply don’t have the right enzymes to break them apart. This means fructans pass untouched through the stomach and small intestine and arrive intact in the colon. That’s where all the problems begin.
As you can expect, fructans are found in fruits. In addition, they also occur in certain vegetables, lots of processed foods, and a handful of beverages.
Do You Have Fructan Intolerance?
Fructan intolerance is tough to diagnose. There are no direct lab tests for it. (Some would say breath testing works. However, breath testing works for fructose, not fructans.)
What the medicos do instead is look at symptoms.
The signs of fructan intolerance are easy to spot:
- Stomach pain
- Gas & bloating
- Constipation and/or diarrhea
- Nausea
- Cramps
That list overlaps with symptoms of gluten sensitivity. (Bone loss is an additional symptom, which isn’t caused by fructans.)
Because they are nearly identical, symptoms of fructan intolerance are often mistakenly diagnosed as gluten sensitivity.
Diagnosing between the two is compounded by foods containing both.
Finding out which type of ingredient might be the perpetrator therefore will take some sleuthing on your part.
It requires doing an N=1 experiment, where you’re the only data point. And the easiest such experiment to conduct on yourself is what’s called an elimination/challenge diet.
It entails executing two scenarios, one after the other:
- Fructan elimination, gluten challenge (i.e., glutens without fructans)
- Gluten elimination, fructan challenge (i.e., fructans without glutens)
Four primary outcomes are possible.
- In the first scenario, symptoms occur if glutens are the cause
- In the second scenario, symptoms occur if fructans are the cause
- If symptoms occur during both scenarios, then fructans and gluten are causal
- If no symptoms occur in either scenario, whatever problems you might have are probably not due to either of these ingredients
How quickly can you see results from this experiment? Published research can help answer that.
One example study (Skodje et al. 2018) showed a very fast response, within 7 days. Subjects in this study were divided into two groups. One group followed scenario #1 for 7 days, while the other group followed scenario #2. They then observed a 7-day washout period, when subjects followed neither scenario (i.e., no fructans or glutens).
After the washout period, the two groups switched scenarios for another 7 days. Switching treatments between the two groups made for what’s called a ‘cross-over’ study. (Your personal experiment will also be a cross-over study, with you as the only subject.)
This is how researchers could determine whether subjects showed sensitivity to either fructans or glutens.
The results were surprising.
They showed fructans to be more likely to induce GI problems than glutens in those reporting sensitivity to the most common high-gluten foods (i.e., wheat, rye, and barley).
This means such gluten-containing foods were not a problem because of their glutens. They were a problem because of their fructans.
The researchers went so far as to suggest their findings weaken the term, non-celiac gluten sensitivity (NCGS), and raise doubts about the need for a gluten-free diet in such cases.
Fructans are now known to be the culprit more often than previously thought. And glutens gets a bad rap more often than they should.
On hindsight, these results point to the supposed benefits of a gluten-free diet being due to fructan elimination, not gluten elimination.
Now, how can you use this information for addressing your own potential for fructan intolerance? And whether you truly need a fructan intolerance remedy?
DIY Testing: How to Conduct An Elimination Diet
Do-it-yourself testing is often easier and more convenient than getting a lab test or medical exam. Cheaper, too.
And doing an elimination diet is perfect for that purpose.
The principle behind elimination diets is simply to remove the potential offender and see what happens to your health.
It relies on making a single change, and keeping everything else the same. Thus, eliminating fructans is the first goal.
Start by eliminating the most common sources of fructans in your diet, which are shown in the following table.
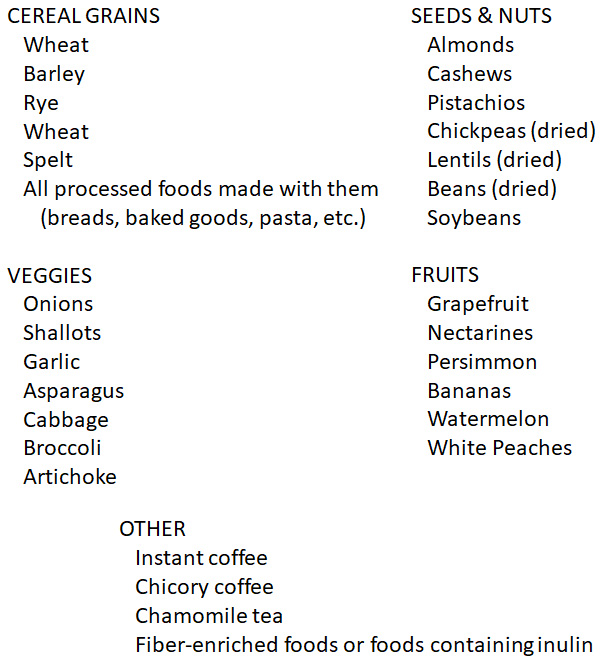
Eliminating wheat products might be the biggest challenge. Wheat is an additive in hundreds of foods. The most obvious include flour-based products. The least obvious can include dry cereals, gravies, meat balls, soy sauce, and gelatinized starch. You really have to read food labels to know for sure.
Once you identify the most likely sources of fructans in your diet, stop consuming them for at least a week. If fructans are causing your problems, then your health should improve noticeably by then.
Wait! There’s More!
Recall that example study I mentioned earlier and do your own equivalent cross-over experiment.
This step is important for distinguishing whether your GI issues are due to fructans or to glutens.
The simplest way to determine that is to eliminate fructans AND glutens to see if you improve. And, if you do, reintroduce fructans without consuming glutens. If your health issues reappear, then fructans are probably driving them.
And Still More!
What happens if your fructan elimination diet doesn’t make you feel better?
Well, this may come across as a disappointment: Other kinds of carbohydrates may duplicate the same symptoms as fructan intolerance.
Yeah, I can guess what you’re thinking – DANG! (To keep it PG-rated, anyway.)
Health professionals now point to a whole group of potential problem ingredients among different kinds of carbs.
As a group, they include carbs characterized by two main features: 1) they’re hard to digest; and, 2) they’re fermentable.
Specifically, they’re certain small-chain carbs (oligosaccharides), two-sugar carbs (disaccharides), single sugars (monosaccharides), and sugar alcohols (polyols).
And it’s a mouthful (sorry, couldn’t resist that one). That’s okay, since the powers that be have created a more easily used acronym for them: FODMAP.
It stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols.
GI specialists have now come up with a low-FODMAP diet as a treatment for intestinal disorders. It’s designed to remove as many fermentable carbs as possible.
The goal of a low-FODMAP diet is to reduce the food sources of colon bacteria whose fermentation by-products include gasses and fatty acids in your gut. The diet is a treatment of choice for irritable bowel syndrome (IBS) and small intestinal bacterial overgrowth (SIBO).
When I first encountered the story about FODMAP issues, I began to wonder what’s the deal with so many types of food ingredients going south on human health.
Good Grief! What CAN You Eat?
Here’s some great news: Foods aren’t the problem. Your gut is.
If your gut worked properly, you could eat the wide variety of foods you’re meant to eat.
Fructan intolerance, FODMAP insanity – even gluten sensitivity – and many more digestive disorders simply wouldn’t exist if your gut were healthy.
This is where mainstream medicine fails miserably. The fundamental reason rests on the failure to even recognize the fundamental cause of the majority digestive disorders: leaky gut syndrome.
A case in point is this typical commentary from the Cleveland Clinic:
Leaky gut syndrome is a theory that intestinal permeability is not only a symptom of gastrointestinal disease but an underlying cause that develops independently. If your intestinal barrier is impaired, it may be letting toxins into your bloodstream. These toxins may trigger an inflammatory response that may manifest as various diseases.
The theory has some appeal as a way of explaining various conditions that we haven’t been able to fully explain yet, but the evidence is lacking. We know that the condition of having intestinal permeability or a “leaky gut” is real, but we don’t know that it’s a disease in itself, or that it causes other diseases. It’s not currently a recognized medical diagnosis. [My bolding.]
This view exemplifies the ‘three monkeys’ approach to chronic human disorders. It’s the ‘we don’t wanna know about it’ strategy behind a studied ignorance of human biology.
If you’re not quite sure what purpose this could have, I’ll invoke my most common answers to a lot of ‘conventional wisdom’ from modern medicine – follow the money.
There’s little to no incentive for addressing a problem with basic biology unless expensive drugs can be developed for treating it.
All the while the best answers lie in acknowledging how the human body works and what to to when it doesn’t work so well.
Solving Your Leaky Gut Puzzle
Knowing about leaky gut syndrome is a good start. My earlier post, Herbs To Heal Leaky Gut, points you in the right direction. And it provides examples of natural treatments for getting your gut biology back on track.
I’m going to go out on a limb here and say this:
Leaky gut syndrome is behind nearly all digestive disorders.
Restoring your GI tract to good health should be the FIRST step toward healing any and all of them.
Fundamentally, restoring gut health requires improving your microbiome – the friendly microbes your GI health depends on.
Starting with understanding one of the most common disruptions of gut health, yeast (candida) overgrowth.
This article should give you some good ideas on what that entails: Ultimate Candida Diet – Foods to Eat, Foods to Avoid.
BOTTOM LINE: Once you heal your leaky gut, which you almost certainly have, you will not need a fructan intolerance remedy in the first place. Or any other superficial gut health remedy, for that matter.
Comments or Questions?
I’d love to hear from you. This and every other post here provides a comment section at the end of the post, exactly for that purpose.
So, by all means, leave me your thoughts.
I would be especially grateful if you point out any flaws in my logic, factual errors, or ordinary typos. (I’ll give you a little ‘huzzah’ in my heart.)
Then I’ll respond as soon as I can.
References
Fedewa A, Rao SS. Dietary fructose intolerance, fructan intolerance and FODMAPs. Curr Gastroenterol Rep. 2014 Jan;16(1):370. doi: 10.1007/s11894-013-0370-0. PMID: 24357350; PMCID: PMC3934501. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3934501/
Laatikainen R, Koskenpato J, Hongisto SM, Loponen J, Poussa T, Huang X, Sontag-Strohm T, Salmenkari H, Korpela R. Pilot Study: Comparison of Sourdough Wheat Bread and Yeast-Fermented Wheat Bread in Individuals with Wheat Sensitivity and Irritable Bowel Syndrome. Nutrients. 2017 Nov 4;9(11):1215. doi: 10.3390/nu9111215. PMID: 29113045; PMCID: PMC5707687. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5707687/
Muir JG, Shepherd SJ, Rosella O, Rose R, Barrett JS, Gibson PR. Fructan and free fructose content of common Australian vegetables and fruit. J Agric Food Chem. 2007 Aug 8;55(16):6619-27. doi: 10.1021/jf070623x. Epub 2007 Jul 11. PMID: 17625872. https://pubmed.ncbi.nlm.nih.gov/17625872/
Pessarelli T, Sorge A, Elli L, Costantino A. The low-FODMAP diet and the gluten-free diet in the management of functional abdominal bloating and distension. Front Nutr. 2022 Nov 8;9:1007716. doi: 10.3389/fnut.2022.1007716. PMID: 36424920; PMCID: PMC9678936. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9678936/
Skodje GI, Sarna VK, Minelle IH, Rolfsen KL, Muir JG, Gibson PR, Veierød MB, Henriksen C, Lundin KEA. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-Reported Non-Celiac Gluten Sensitivity. Gastroenterology. 2018 Feb;154(3):529-539.e2. doi: 10.1053/j.gastro.2017.10.040. Epub 2017 Nov 2. PMID: 29102613. https://pubmed.ncbi.nlm.nih.gov/29102613/
Kinashi Y, Hase K. Partners in Leaky Gut Syndrome: Intestinal Dysbiosis and Autoimmunity. Front Immunol. 2021 Apr 22;12:673708. doi: 10.3389/fimmu.2021.673708. PMID: 33968085; PMCID: PMC8100306. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8100306/
Laatikainen R, Koskenpato J, Hongisto SM, Loponen J, Poussa T, Huang X, Sontag-Strohm T, Salmenkari H, Korpela R. Pilot Study: Comparison of Sourdough Wheat Bread and Yeast-Fermented Wheat Bread in Individuals with Wheat Sensitivity and Irritable Bowel Syndrome. Nutrients. 2017 Nov 4;9(11):1215. doi: 10.3390/nu9111215. PMID: 29113045; PMCID: PMC5707687. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5707687/
All the best in natural health,
![]()
Statements on this page have not been evaluated by the Food and Drug Administration. Information here is not is not intended to diagnose, treat, cure, or prevent any disease.
I may receive a commission for purchases made through those links.
This doesn’t change the cost to you.
Leave a Reply