 When it comes to insulin resistance and diabetes, everyone agrees that eating right is vital for good health management of diabetes. If you don’t know what that means, then you will not recognize the bad dietary advice coming from mainstream medicine.
When it comes to insulin resistance and diabetes, everyone agrees that eating right is vital for good health management of diabetes. If you don’t know what that means, then you will not recognize the bad dietary advice coming from mainstream medicine.
Reversing Insulin Resistance
Yes, eating right can overcome insulin resistance and reverse diabetes.
The sooner the better.
This is where general agreement ends and arguments about what ‘eating right’ means. Indeed, the old name of ‘sugar diabetes’ for type 2 diabetes has long been called into question. Long-term consumption of sugar is still associated with development of the disease. However, it is the production and function of insulin that seems to explain more about what goes wrong leading up to diabetes. It also explains several other diseases of modern civilization.
Fueling the Fire
As most people already know, insulin, a hormone produced by the pancreas, enables the body’s cells to absorb glucose (blood sugar). On the road to diabetes, however, cells start losing their ability to respond properly to insulin. This is called insulin resistance.
In response to insulin resistance, the body produces even more insulin to deal with excess blood sugar. Blood sugar and insulin levels both increase. The end point is an overtaxed pancreas that finally gives out and fails to produce any insulin at all.
As this end point is approached, insulin and blood sugar increasingly cause serious damage to many tissues. And it all began with too much dietary carbohydrate that induced overproduction of insulin in the first place.
Insulin is a crucial hormone for good health. Too much insulin, however, is highly inflammatory. It will ruin your health in many ways.
The Insulin Connection to Disease
Abnormal metabolism of insulin lies at the root of diabetes, high blood pressure, elevated triglycerides, heart disease, and obesity. The greater intake of carbohydrates that stimulate insulin, the greater the levels of insulin, the greater the occurrence of these diseases. If a picture is worth a thousand words, this is what insulin production looks like with and without insulin resistance.
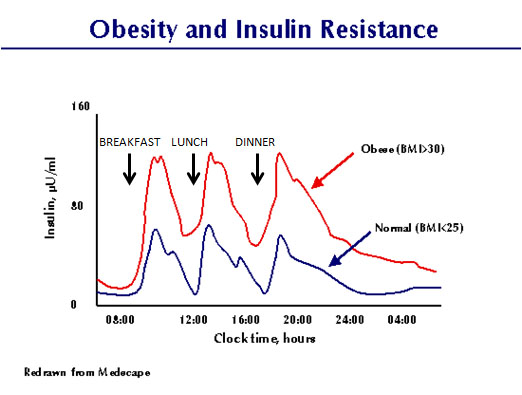
The pancreas responds to a meal by producing a spike of insulin, after which insulin returns to a between-meal level. Notice that the spike is much higher, and stays high even between meals, when cells are insulin resistant (such as in obesity).
To limit damage by excess insulin, it is beneficial for a diabetic (and everyone else) to limit carbohydrate intake. This is how to reduce the amount of blood sugar that leads to too much insulin and the development of insulin resistance.
Now for Some Bad Advice
Let’s just pick on one doctor who exemplifies the bad advice handed out to diabetics regarding diet. The only reason for singling out this particular doctor is because he and his advice for diabetics were prominently featured in a recent issue of the AARP magazine, Special Health Issue (Oct/Nov 2014). However, it represents the party line for mainstream medicine that comes from many, many other doctors.
The doctor of note is George King, MD, who is the Director of Research and Head of the Section on Vascular Cell Biology at the Joslin Diabetic Center in Boston, as well as a Professor of Medicine at Harvard Medical School. Seems like a super-qualified source for health advice, right? Let’s see. In the article mentioned here, Dr. King offered the following 7 steps as the ‘best tactics for fighting the blood sugar disease’.
Step 1: Cut the fat, up the fiber. Specifically, the ideal diet consists of 15 percent fat, 15 percent protein, and 70 percent carbohydrates.
Hold that thought for a moment. Overproduction of insulin is at the root of diabetes and several related inflammatory diseases. Carbohydrates become blood sugar that stimulates insulin production. Hmm. Houston, we have a problem.
The challenge for diabetics and everyone else is to keep insulin levels under control. Let’s take a look at a relatively simple study published way back in 1996 that shows how to do that. This is a rare study in that it involved patients in a hospital setting where every last smidgeon of food was controlled and kept track of. Here is what the summary graph of food intake looks like:
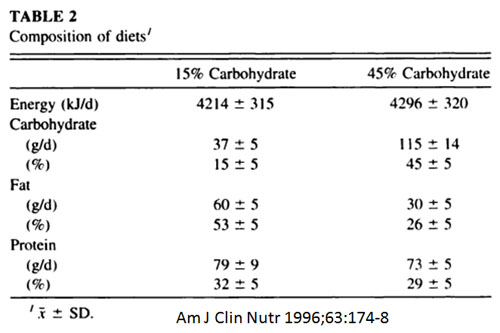
The ‘Energy’ component translates into about 1,000 Calories per day, so this represents a low-calorie diet. It is a variable that confounds certain interpretations of the results, but we are stuck with it. Nevertheless, the two groups of experimental subjects represent ‘low’ carbohydrate (15 percent) and ‘high’ carbohydrate (45 percent) diets.
Although the study focused on changes in weight and body composition after 6 weeks, the most telling result was the comparative influence of each diet on insulin levels. The graph of this result (indicated by the added red arrows) showed the following:
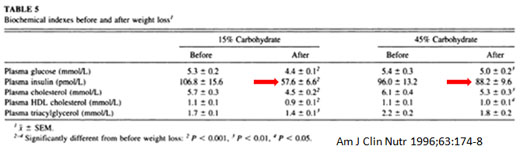
Although this table looks a little fuzzy due to technical issues with image reproduction, it shows a drop in insulin of about 8 percent with the high-carb diet vs. about 46 percent on the low-carb diet.
Low-carb eating controls insulin levels better than high-carb eating, by a factor of almost 6-fold! Wow!
Keep in mind that the ‘high’ carbohydrate diet is 45 percent of intake in this study and that Dr. King recommends this to be 70 percent for diabetics.
We can debate the merits of this study all day long, and even throw in a bunch of other studies that compare changes in weight and body composition in response to different diets. The bottom line, though, is that low-carb eating controls insulin levels and high-carb eating is like adding gasoline to a fire.
Note also that Dr. King’s advice is low-fat, even though fat is the only food group that has no impact on insulin levels.
The advice about fiber is a little better, although the reason is that ‘fiber makes you feel full more quickly and helps you absorb calories more slowly’. This comment ignores the observations by others that satiety depends more on eating protein and fat. Oh, and absorbing calories at all is a biochemical and physical misconception. Almost everyone gets this wrong. Measuring food intake based on its calorie potential is simply idiotic.
What About the Other 6 Steps?
Here they are in a nutshell, with a bit of added commentary.
Step 2. Don’t rely on supplements. “…food works and supplements don’t.” This is typical medical arrogance. Don’t get me started.
Step 3. Get 6-8 hours of sleep nightly. Finally, a piece of good advice!
Step 4. Calm yourself. Great idea for everyone, although exactly how to do so is not included with Dr. King’s instructions.
Step 5. Stop being a weekend warrior. The explanation here advocates exercise. It is another great idea with mostly missing ‘how-to’.
Step 6. Exercise in a cold gym. Good luck with that. The concept behind this advice is based on activating so-called brown fat. Experiments to do so suggest that any significant change in brown fat activity requires ice and lots of it. Merely exercising in a cold gym is inadequate.
Step 7. Ask about new meds. This is, of course, the mainstream medical party line. In this case, the Avandia ‘scandal’ may also be behind this advice. Avandia and similar insulin sensitizers (Rezulin, Actos) have serious side effects, including liver damage, heart attack, stroke, and heart failure. Rezulin was recalled in 2000, Avandia was placed under severe restriction in 2010 (since lifted by the FDA!), and Actos has been repeatedly linked to heart failure and bladder cancer. Go ahead and ask about new meds if you wish, but the track record on old meds does not bode well for new replacements.
All in all, Dr. King’s advice is either just plain bad or falls short of being helpful.
All the best in natural health,
![]()
Statements on this page have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
Is insulin a fat pill? I have gained fat because my diabetes doctor increases my insulin. If diabetes is reversed by losing weight, why do doctors prescribed insulin?
Hi, Felipe…Yes, the continued use of insulin can make you fat. The reason doctors prescribe it is because it is a simple-minded fix for a complex problem that arose from lifestyle choices (diet, etc.). Oh, and Big Pharma makes a lot of money this way. You will never recover your health by taking increasing doses of insulin. It is a downward spiral to poor health. Working with a good naturopathic doctor would no doubt be helpful to you.
All the best,
Dennis