
I’m not sure how many more body parts I can lose and still be above ground. Now those chilling words from my doctor, “That sucker has got to go!,” (or words to that effect) includes one more – my gallbladder. This post is about how I got to this point, and what I (and others) must do to be healthy after losing my little bile-storing buddy.
Why I’m Writing This Post
Two main reasons:
1) Whenever I’m facing a new ‘health adversity’, writing about it is therapeutic.
2) I want to educate others about what to expect after gallbladder removal, with a strong dose of science behind it. Hopefully this helps cut through all of the often contradictory blather online about gallbladder-free living.
Now dig in and see what you think.
Some Really Scary Sh*t
At the beginning of 2025 I had what seemed like an intestinal blockage, which landed me in the ER. This normally comes with the territory from the ‘replacement’ colon I got back in 1991. (It’s called a J-pouch, which substitutes for an external ostomy bag. That’s another story.)
This time a CAT scan showed no blockage. Instead it showed a ‘mass’ in my gallbladder, measuring 4.2 x 3.0 x 7.2 cm. That mass is almost as large as a typical gallbladder (i.e., 7-10 cm x 3-4 cm).
SIDENOTE: The ER doc recommended that I also get a follow-up ultrasound. Talk about duplication of effort. You want to know what it showed? A mass in my gallbladder. Sheesh!
Sooo…my gallbladder is comprised almost entirely of an unknown, sludgy mass of who-knows-what. Nobody can tell me what it is for certain. Fear of the unknown is real, so this uncertainty really ramped up my ‘scary-sh*t index‘.
That was the beginning.
In a post-op visit with my doc from an earlier surgery, Dr. Erin Kloos, she asked me what else she could do for me. I casually mentioned my gallbladder issue, which led her to order an immediate MRI.
The results repeated those of earlier scans, with the addition of words nobody wants to hear: “…highly suspicious of malignancy.”
AW, CRAP!
My first inclination was to be conservative, to see whether I could shrink that mass with dietary changes and supplements. All that’s now changed.
That’s because I found that, although gallbladder cancer is rare, when it does occur it’s disastrous.
According to cancer.org, gallbladder cancer is not usually found until it has become advanced and causes symptoms. Only about 1 of 5 gallbladder cancers is found in the early stages, when the cancer has not yet spread outside the gallbladder. Yet when it spreads in later stages, the 5-year survival rate drops off a cliff. (This is typical for metastasizing cancers in general.)
My symptoms? Nausea, projectile vomiting, explosive diarrhea – all at the same time. (Maybe I should have warned you about that grossness ahead of time? Too late now.)
All clearly explained by a hinky gallbladder.
As is my constant feeling of ickiness in my gut. (‘Ickiness‘ is my technical term for low-level nausea.)
BOTTOM LINE: My gallbladder is now scheduled for removal. Dr. Kloos will be my surgeon once again. My first surgery by her – hernia repair – went so well that I told her I’d be coming back for another one. (After all, if she were a chef, she’d know the best compliment to a chef is when someone comes back for seconds.)
This will be followed by a bon-voyage ceremony for it with some friends sometime afterwards.
Challenges of Gallbladder-Free Living
Although many doctors (and a few other folks) will tell you the gallbladder isn’t important, that’s complete misinformation. It’s not there for nothing.
Among other things, the gallbladder…
- Releases massive amounts of a hormone called cholestykinin (CCK) made in the duodenum; it’s responsible for stimulating the digestion of fat and protein.
- Concentrates and stores bile from the liver, in preparation for digesting food.
- Sequesters wastes and toxins in bile, including LDL cholesterol.
- Absorbs fat-soluble vitamins (i.e., A, D, E, and K2).
- Reduces risks of malignancies such as leukemia and cancers of the colon, liver, pancreas, biliary tract, thyroid, pharynx, and oral cavity. (See the reference below by Choi et al. 2022.)
These are not trivial functions!
The challenge is to make up for those changes once the gallbladder gets yanked out.
Plenty of diseases can be tied to the absence of a gallbladder, including the cancers mentioned above. Many other issues can arise due to deficiencies in the fat-soluble vitamins.
For example, the role of vitamin K2 in cardiovascular health is critical, although underappreciated (Hariri et al. 2021). One immediate concern after gallbladder removal is cardiovascular disease (Chavez-Tapia et al. 2021, Kim et al. 2021). It may only be a short-term issue (ca. 2 years), depending on vaguely defined improvements in ‘metabolic health’ after gallbladder removal (Park et al. 2024). Nevertheless, I expect that this issue is best explained by diminished levels of vitamin K2.
These and all those other reduced-function issues listed above will form the basis for how I intend to address my newfound challenges.
Action Steps for Living Without a Gallbladder
General advice about gallbladder-free living focuses on diet, which is a good start. However, most such advice is pretty namby-pamby.
The biggest concern is diarrhea. In the absence of meal-induced release of stored bile from a gallbladder, bile from the liver continuously ‘leaks’ directly into the small intestine. This often leads to constant diarrhea. Add that to my already loosey-goosey stools from the lack of a colon, and I’m expecting what I would call turbodiarrhea. This will probably be my biggest challenge.
Here’s what the Mayo Clinic has to say about it: Can you recommend a diet after gallbladder removal? (with my comments in bold).
The bottom line advice is:
- Go easy on the fat. Don’t eat high-fat foods, fried and greasy foods, and fatty sauces and gravies for at least a week after surgery. Instead, choose fat-free or low-fat foods. Low-fat foods are those with no more than 3 grams of fat in a serving. Check labels and follow the serving size listed. MY COMMENT: This may be advisable temporarily, while still recovering from surgery. However, it completely violates how humans evolved to eat. It specifically ignores how we developed such a big brain based on dietary fat (especially DHA and EPA from marine sources). We evolved as top carnivores, not vegetarians. See my earlier post on that topic here: The Real Paleo Diet Made You a Brainiac.
- Increase the fiber in your diet. This can help make bowel movements more regular. Add soluble fiber, such as oats and barley, to your diet. But be sure to increase the amount of fiber slowly, such as over several weeks, because too much fiber at first can make gas and cramping worse. MY COMMENT: This is pretty good advice, although those fiber sources aren’t so hot. The best ‘bulking’ fiber I’ve found (and already use daily) is psyllium seed husk powder (e.g., Psyllium Husk from Source Naturals; many other brands also offer this product).
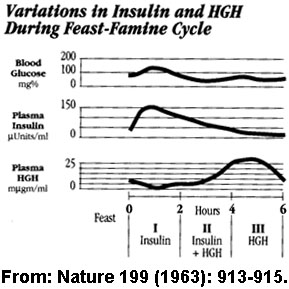
- Eat smaller, more frequent meals. This may ensure a better mix with available bile. A healthy meal should include small amounts of lean protein, such as poultry, fish or fat-free dairy, along with vegetables, fruits and whole grains. MY COMMENT: This advice is wrong in so many ways. Sure, eating smaller meals more often may help reduce gallbladder-free diarrhea. Unfortunately, it will keep your insulin levels chronically high and your hGH (growth hormone) levels chronically low. We’ve known the value of proper meal spacing at least since 1963 (although many dieticians seem to be unaware of it). This is what’s supposed to happen when meals are spaced appropriately:
Frequent small meals undermine the power of short-term fasting (4-5 hours) between meals.Furthermore, eating too often slows down autophagy – our cellular garbage removal system – by overloading it with too much dietary junk. This in turn upsets the balance between autophagy and apoptosis (aka, “programmed cell death”), which creates massive amounts of cellular debris from old dead cells. This can stymie new cell production.]
Although eating smaller meals more frequently may be a short-term strategy for adjusting to life without a gallbladder, long-term it’s the wrong way to eat.
- Also try limiting foods that tend to worsen diarrhea, including: caffeine, dairy products, very sweet foods. [MY COMMENT: Dairy, sure. Caffeine, not so sure. Very sweet foods – too vague. I’d simply cite the general value of avoiding highly processed foods containing sugar or quickly-digested carbs.]
BONUS COMMENT ABOUT DIETARY ADVICE: As I mentioned earlier, dietary advice is pretty namby-pamby. Nevertheless, diet seems to be the focus on many, many clinic sites. And it’s almost always the same, such as that as outlined above from the Mayo Clinic. However, get a load of this quote from Dahmiwal et al. (2024): The findings from the conducted studies suggest that, although dietary changes are a common recommendation, these measures are not sufficiently supported by evidence when it comes to alleviating symptoms and improving outcomes post-cholecystectomy.
So this leaves me exactly where? Well, as is often the case, I’ll have to figure it out on my own, with a heavy dose of consultation with my friend, Dr. Melonni Dooley, ND. She is a brilliant naturopathic doctor who has helped me and many others over the years with her insights into natural approaches to health (see: https://solutionsforlifenaturally.com/).
After a healing period of days or weeks on a bland, mostly liquid diet, I’ll start out by upping my intake of psyllium powder. Supplementing with ox bile salts may also be helpful. So I’ll experiment with one of those, such as this one: https://doublewoodsupplements.com/products/ox-bile-acid-salts.
What can I do about these missing functions I will be facing? Here’s a start.
About CCK
I won’t benefit from its role in gallbladder function, so that’s off the table. In fact, my duodenum may make more of it, which stimulates the production of more bile. This is one reason why lack of a gallbladder leads to diarrhea. I still need plenty of CCK, since it’s widespread in other areas of the body. For example, it’s the most abundant neuropeptide in the central nervous system. So I’m not going to do anything to slow its production down.
About Bile Storage
I won’t have bile storage anymore. It will be off to the races with bile going directly from my liver to my small intestine. Nothing to do about this issue except slow it down with psyllium husk powder. It will take some experimentation to learn how much and how often I need to do this.
About Toxin Elimination
Probably the most reported-on issues here involve the potential for developing metabolic syndrome (Di Ciaula et al. 2018). One concern arises from the gallbladder’s role in maintaining lipoprotein levels (especially LDL cholesterol). Metabolic syndrome is also tied to diabetes and obesity. I’m not at all worried about these issues, since I already have a good handle on how to handle the key indicators: my weight is perfect, my cholesterol levels are ideal, and my fasting blood glucose and HbA1c levels are low. I’ll just monitor them to make sure nothing goes awry. At this time, I believe there is very little chance I will ever have problems with any of those.
About Fat-Soluble Vitamins
This may have a simple solution – just take higher amounts of those vitamins. I already take a K2 supplement, so I’ll look into A and E supplements.
As far as vitamin D goes, I’ve boosted my levels over the years by simply sunbathing in the middle of the day. This is when UVB light in the solar spectrum maxes out. That’s the only energy source humans can use for making vitamin D in our skin. Specifically, UVB light drives the sulfation of a modified cholesterol to form vitamin D3 sulfate.
That is the key form of vitamin D that gets transported to every cell that has vitamin D receptors (VDRs) – which is just about every cell in the body. (By the way, making a substance in one place and sending it to a receptor in another place is the classic definition of a hormone. Indeed, that’s what vitamin D actually is [meaning, not really a vitamin].)
My strategy has already raised my natural vitamin D level, from 37.7 ng/mL in 2011 to 65.9 ng/mL in 2023. (For comparison, 30 ng/mL is considered to be the low end of acceptable.) So I’m already good there. I’ll just have to keep monitoring it to be sure it doesn’t drop.
Vitamin D supplements could also help, although supplemental vitamin D3 isn’t as effective as the one we make. (NOTE: There are no vitamin D3 sulfate supplements.]
About the Risk of Cancer
The Warburg effect generally rules the development of cancer. Biochemically, it relies on dysfunctional glucose metabolism. As long as I keep my blood sugar levels low, this should not be a problem. My diet already accounts for that, so I’m good here.
Although Otto Warburg first outlined the effect in the 1930s, his early 20th century explanation of it was based entirely on the biochemistry of the day. It turns out that it’s really a bioelectrical dysfunction, since mitochondrial metabolism is essentially an electron flow process. In other words, it’s a biophysics problem, not a biochemical problem. Just sayin’.
More critically, the Warburg effect rests on mitochondrial energy dysfunction. Undermining the effect demands having electrically healthy mitochondria, which I also have a good handle on. (See my earlier post about it here: Live Long And Prosper With Healthy Mitochondria.)
In a more practical sense, anti-cancer mitochondrial function depends stem cells (Martinez et al. 2024), which can be addressed therapeutically (Baghli et al. 2024). The latest therapy, as detailed in that article by Baghli et al., is pretty simple and inexpensive relative to treatments by mainstream medicine.
Therefore, I will be boosting my already anti-cancer lifestyle with the protocol described in that article. If cancer is a bugaboo linked to gallbladder removal, it won’t stand a chance with me!
One More Thing
As I was looking around for research on the consequences of gallbladder removal, I found a study that surprised me. McDonnell et al. (2002) stated that, “This study suggests that cholecystectomy causes an exaggerated meal-stimulated CCK response. Because CCK is known to relax the lower esophageal sphincter, these findings may help explain the increased incidence of gastroesophageal reflux seen after cholecystectomy.”
Oh, goodie. Heartburn on the horizon.
This has never been a problem for me. If it happens, I’ll explore upping my use of digestive enzymes (with betaine HCl), apple cider vinegar, and bitter herbs such as chicory and gentian. These are all well-known digestive aids that might help keep that lazy esophageal sphincter out of play.
In addition, I will no doubt start supplementing with ox bile salts (e.g., https://www.amazon.com/Gallbladder-Standardized-Deficiencies-Double-Wood/dp/B0CBKXX1W5/). This supplement specifically helps digestion in the absence of a gallbladder.
All this will allow me to re-acclimate to my usual high-fat diet. Fat is so valuable for good health that limiting its intake is a non-starter for me. I may have to slowly reintroduce fats into my diet over time to make up for the absence of my missing little fat-digester.
One thing that I will never do is take antacids. The whole concept behind antacids is just about as stupid as it can be. GERD isn’t caused by excess stomach acid. It’s caused by stomach acid bubbling up through the esphageal sphincter. We NEED plenty of stomach acid for good digestion.
The Adventure Begins…
As of this writing (3/24/2025), my surgery is scheduled for two weeks from now.
I’ve already learned a lot about what to expect afterwards. Onlinr vomments by many others about their experiences with gallbladder-free living are all over the map. What my experience will be is going to be a work in progress.
Anything I discover or decide to do will be based on published scientific research and consultation with my naturopathic doctor, Dr. Melonni Dooley (mentioned earlier). My first choice out of the blocks always focuses on natural approaches to health.
Discovering whatever works or doesn’t work will be an ongoing experiment. I will add new developments to the comments section below when I have found something useful.
Keep in mind that my digestion is different from most people’s, unless they’ve also lost the colon to the Samurai Surgeon as I have. One advantage I have is getting digestive results in a hurry. When the colon is gone, transit time through the GI tract is like NASCAR races. Very fast. That means I don’t own my food so much as rent it. What a perk, huh?
Comments or Questions?
I’d love to hear from you. This and every other post here provides a comment section at the end of the post, exactly for that purpose.
So, by all means, leave me your thoughts.
I would be especially grateful if you point out any flaws in my logic, factual errors, or ordinary typos. (I’ll give you a little ‘huzzah’ in my heart.)
Then I’ll respond as soon as I can.
References (for other nerds like me)
Baghli I, Makis W, Marik PE, , Gonzalez MJ, Grant WB, Hunninghake R, Levy TE, Lim H, Cheng RZ, Bondarenko I, Bousquet P, Ortiz R, Mary M, D’Agostino DP, Martinez P . Targeting the Mitochondrial-Stem Cell Connection in Cancer Treatment: A Hybrid Orthomolecular Protocol. J Orthomol Med. 2024. 39.3. https://isom.ca/article/targeting-the-mitochondrial-stem-cell-connection-in-cancer-treatment-a-hybrid-orthomolecular-protocol/
Chavez-Tapia NC, Kinney-Novelo IM, Sifuentes-Rentería SE, Torres-Zavala M, Castro-Gastelum G, Sánchez-Lara K, Paulin-Saucedo C, Uribe M, Méndez-Sánchez N. Association between cholecystectomy for gallstone disease and risk factors for cardiovascular disease. Ann Hepatol. 2012 Jan-Feb;11(1):85-9. PMID: 22166565. https://www.sciencedirect.com/science/article/pii/S1665268119314905
Dahmiwal T, Zade A, Tote D, Reddy S, Sudabattula K. Dietary Considerations in Cholecystectomy: Investigating the Impact of Various Dietary Factors on Symptoms and Outcomes. Cureus. 2024 May 27;16(5):e61183. doi: 10.7759/cureus.61183. PMID: 38933619; PMCID: PMC11200314. https://www.cureus.com/articles/257531-dietary-considerations-in-cholecystectomy-investigating-the-impact-of-various-dietary-factors-on-symptoms-and-outcomes#!/
Di Ciaula A, Garruti G, Wang DQ, Portincasa P. Cholecystectomy and risk of metabolic syndrome. Eur J Intern Med. 2018 Jul;53:3-11. doi: 10.1016/j.ejim.2018.04.019. Epub 2018 Apr 26. PMID: 29706426; PMCID: PMC8118133. https://pmc.ncbi.nlm.nih.gov/articles/PMC8118133/
Hariri E, Kassis N, Iskandar JP, Schurgers LJ, Saad A, Abdelfattah O, Bansal A, Isogai T, Harb SC, Kapadia S. Vitamin K2-a neglected player in cardiovascular health: a narrative review. Open Heart. 2021 Nov;8(2):e001715. doi: 10.1136/openhrt-2021-001715. PMID: 34785587; PMCID: PMC8596038. https://pmc.ncbi.nlm.nih.gov/articles/PMC8596038/
Kim YJ, Park YS, Shin CM, Han K, Park SH, Yoon H, Kim N, Lee DH. Risk of Heart Disease after Cholecystectomy: A Nationwide Population-Based Cohort Study in South Korea. J Clin Med. 2021 Jul 23;10(15):3253. doi: 10.3390/jcm10153253. PMID: 34362037; PMCID: PMC8348353. https://pmc.ncbi.nlm.nih.gov/articles/PMC8348353/pdf/jcm-10-03253.pdf
Martinez P, Baghli I, Gourjon G, Seyfried TN. Mitochondrial-Stem Cell Connection: Providing Additional Explanations for Understanding Cancer. Metabolites. 2024 Apr 17;14(4):229. doi: 10.3390/metabo14040229. PMID: 38668357; PMCID: PMC11051897. https://www.mdpi.com/2218-1989/14/4/229
McDonnell CO, Bailey I, Stumpf T, Walsh TN, Johnson CD. The effect of cholecystectomy on plasma cholecystokinin. Am J Gastroenterol. 2002 Sep;97(9):2189-92. doi: 10.1111/j.1572-0241.2002.05971.x. PMID: 12358231. https://journals.lww.com/ajg/abstract/2002/09000/the_effect_of_cholecystectomy_on_plasma.12.aspx
Park S, Jeong S, Park SJ, Song J, Kim SM, Chang J, Choi S, Cho Y, Oh YH, Kim JS, Park YJ, Son JS, Ahn JC, Park SM. Associations of cholecystectomy with metabolic health changes and incident cardiovascular disease: a retrospective cohort study. Sci Rep. 2024 Feb 8;14(1):3195. doi: 10.1038/s41598-024-53161-6. PMID: 38326522; PMCID: PMC10850095. https://pmc.ncbi.nlm.nih.gov/articles/PMC10850095/
All the best in natural health,
![]()
Statements on this page have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.
Leave a Reply